Your member ID card
When you sign up for health insurance, your health plan will send a member identification (ID) card to you and your covered family members. Your member ID card (or health plan ID card) is proof that you have health insurance. Health care providers use the information from your member ID card to confirm they are part of your plan’s network and to bill your health plan for your care. Some plans have mobile apps that let you share the member ID card on your smartphone or tablet. Keep your member ID card handy when you:
- Go to the doctor
- Go to the hospital
- Have lab work done
- Get a prescription filled (if your plan has drug coverage)
Sign in to get a digital member ID card
- Plan through your employer
- Medicare plan
- Medicaid plan
- See more sign in options
View your member ID card using the UnitedHealthcare app
Use your mobile device to download the UnitedHealthcare app to easily view a digital member ID card, anytime.
Use your mobile device to download the app
You can also sign in to your member account to view a member ID card.

Request a new member ID card
If your card is damaged, or if you find a mistake on your member ID card, call the number on your card to request a new card. If you have lost your member ID card, contact us.
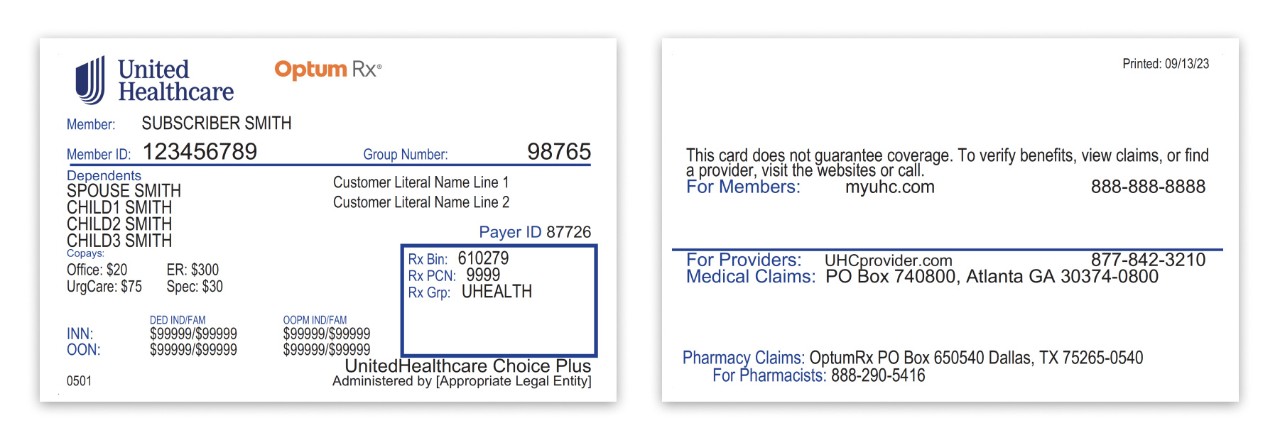
Examples of information found on member ID cards
Here are some examples of UnitedHealthcare member ID cards. Your member ID card may vary depending on your specific health plan and coverage.
Members with insurance through your employer
Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims.
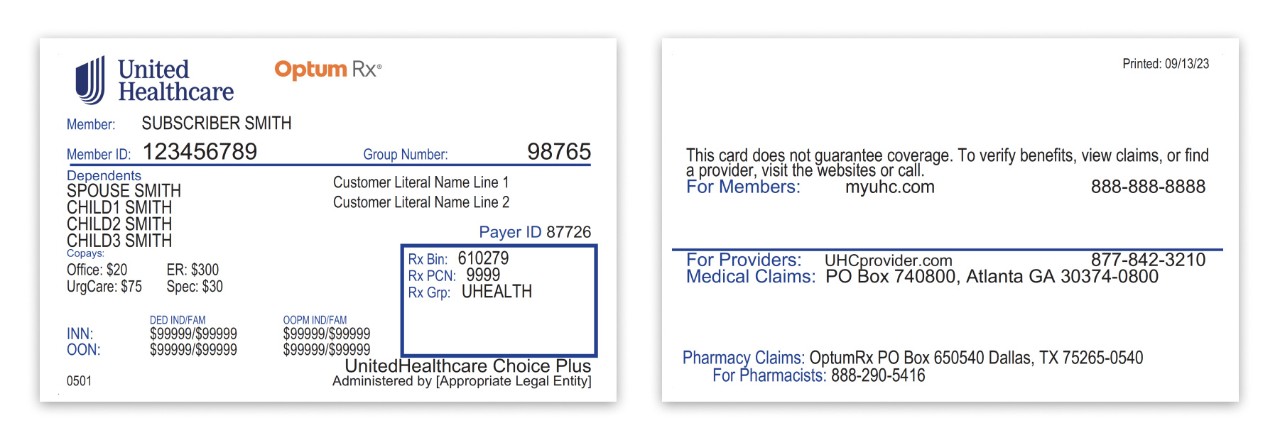
- Member ID number: A unique member ID number that links to your specific health insurance benefits and coverage.
- Group number: This number is unique to your company and is the same for all employees who participate in the insurance plan.
- Member/dependents: Your name (if you’re the policyholder) and other family members covered under your health plan.
- PCP: Primary Care Provider. Some plans require members to choose a primary care provider (PCP). If required, your PCP will be listed on your member ID card. A PCP is your main point of contact for most health issues or concerns. It can be a licensed physician, nurse practitioner, clinical nurse specialist or physician assistant.
- Copay: If your plan has copays, the copay for certain services may be listed on your member ID card. Your copay is the fixed amount you pay for certain covered health care services. It is usually paid when you receive the service.
- Your network: Before selecting a primary care provider (PCP), check that they are in your plan network. You can call the service number on your member ID card, or sign in to your member account and search the provider directory.
- Referrals required: If this appears on your card, check your benefit plan documents to see which services may require a referral (or recommendation) from your PCP for medical care beyond what your PCP can provide.
- Pharmacy benefits: If your plan includes pharmacy benefits from OptumRx®, your member ID card lists the numbers your pharmacy will need to verify your insurance coverage when filling prescriptions.
The back of your UCard includes contact information for providers and pharmacists to submit claims. It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more.
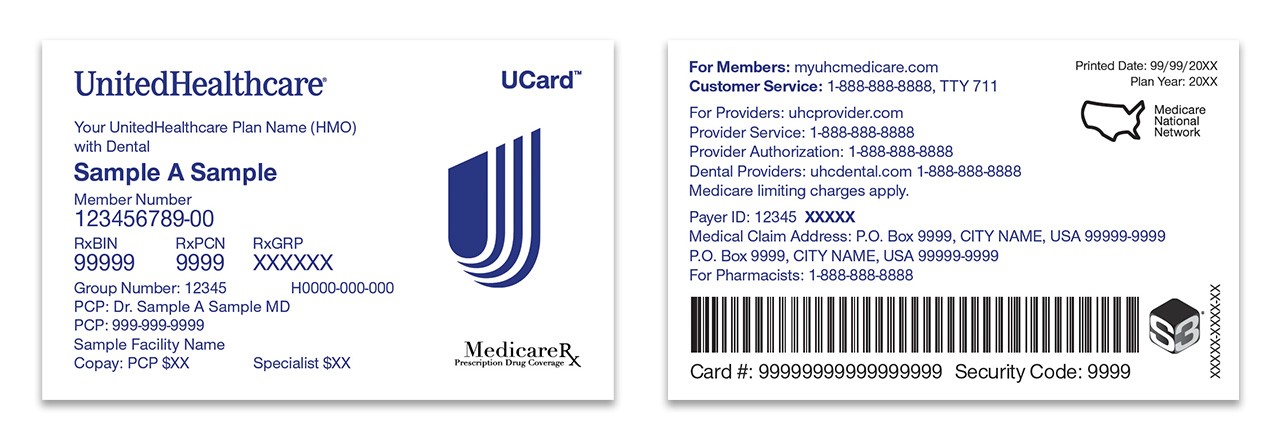
Medicare members
UnitedHealthcare UCard™
Your UnitedHealthcare UCard™ is your member ID — and much more. It makes it easier to access your benefits and programs, so you can take advantage of what your plan has to offer.
Reach for your UCard when you:
- Check in at your provider
- Fill a prescription
- Buy healthy foods, over-the-counter (OTC) products and utilities with your card benefit
- Go to the gym
- Spend your earned rewards
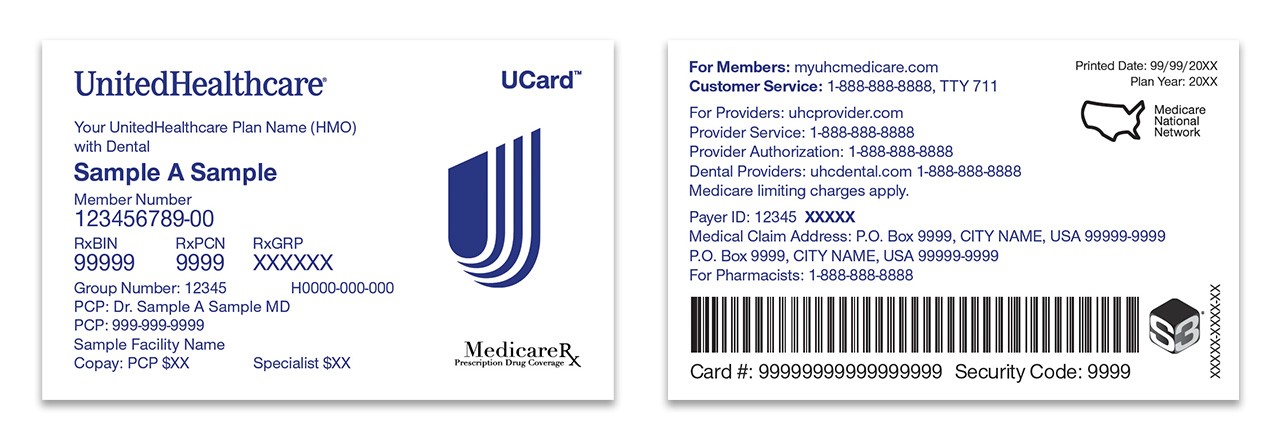
Understanding the numbers on your UCard
A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims.
- Member ID number: Each member has a unique member ID number linked to their specific health insurance benefits and coverage.
- Group number: This number is the same for everyone who participates in that insurance plan.
- Member: Your name
- PCP name: Primary Care Provider. Some plans require members to choose a primary care provider (PCP). If required, your PCP will be listed on your member ID card. A PCP is your main point of contact for most health problems or concerns. It can be a licensed physician, nurse practitioner, clinical nurse specialist or physician assistant.
- PCP phone number: Phone number for you to easily call your primary care provider.
- Copay: If your plan has copays, the copay for certain services may be listed on your member ID card. Your copay is the fixed amount you pay for covered health care services. It is usually paid when you receive the service.
- Pharmacy Benefits: If your plan includes prescription drug coverage, your pharmacy will need to see your member ID card to verify your insurance coverage when filling prescriptions.
- Medicare limiting charges apply: When doctors don’t accept Medicare but haven’t opted out entirely, the most they can charge is 15% over what Medicare will pay for that service (in addition to out-of-pocket costs). Limiting charges do not apply to medical equipment or supplies.
The back of the member ID card includes the member website and phone numbers to connect with customer service, speak with a nurse and discuss behavioral health. It also includes contact information for providers and pharmacists to submit insurance claims.
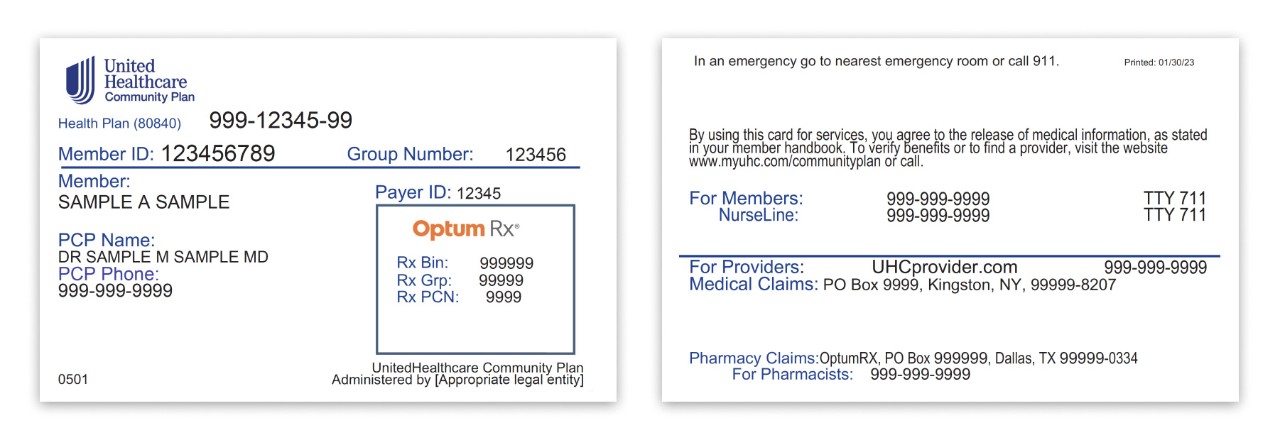
Medicaid/UnitedHealthcare Community Plan members
A member ID number and group number let healthcare providers verify your coverage and file claims for health care services. It also helps UnitedHealthcare advocates answer your questions if you call about benefits and claims.
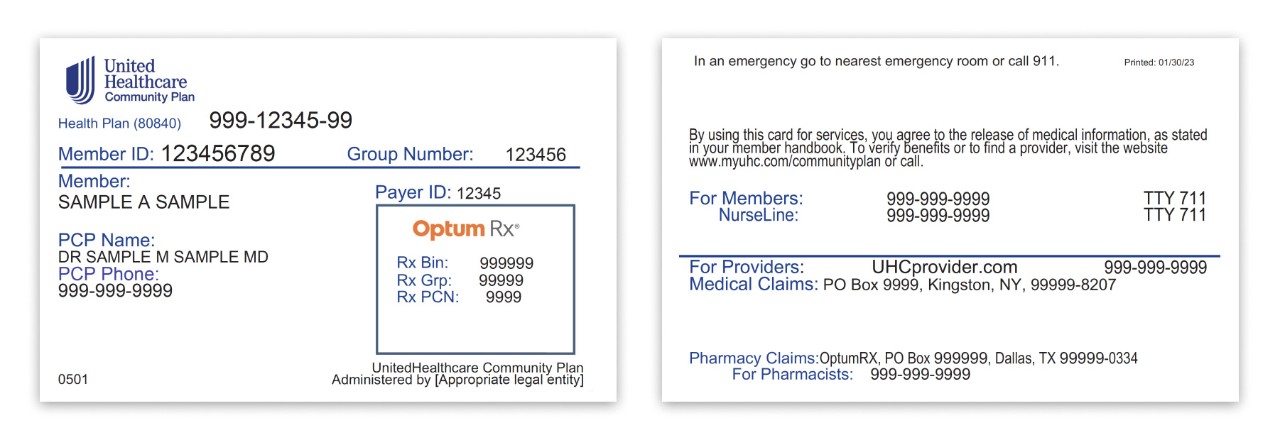
- Member ID number: Each policy holder has a unique member ID number that links to your specific health insurance benefits and coverage. For some members, a unique State ID may also be present on the member ID card.
- Group number: This number is the same for everyone who participates in that insurance plan.
- Member: Your name
- PCP name: Primary Care Provider. This is your main point of contact for most health problems or concerns. It can be a licensed physician, nurse practitioner, clinical nurse specialist or physician assistant. Not all member ID cards contain this information.
- PCP phone number: Phone number for you to easily call your primary care provider.
- Pharmacy Benefits: When your plan includes pharmacy benefits, your pharmacy will need to verify your coverage when filling prescriptions.
The back of the member ID card may include phone numbers to connect with customer service, speak with a nurse and find behavioral health support. It also includes contact information for providers and pharmacists to submit claims.
Preventing medical identity theft
Unfortunately, new health care fraud and abuse schemes are constantly occurring. Thankfully, they are also regularly uncovered. You can help protect yourself and your family by staying informed.
Consider these tips to help safeguard your personal information:
- Treat your member ID card as you would a credit card
- Never provide personal information, such as your member ID number, credit or debit card number (or other personal information) on a phone call you did not initiate
- Do not let anyone except your physician’s office or pharmacy handle your member ID card. If anyone else requests your personal information, do not provide it.
- Never accept “free” medical equipment or services in exchange for your member ID number
- Shred financial documents before discarding
- Monitor your financial accounts regularly